The medical profession has known about the relationship between cancer treatments and cardiotoxicity for many years. It wasn’t long after that relationship was established that a whole new subspecialty of cardiology was founded. It’s called cardio-oncology and its main focus is not just heart failure, but encompasses the entire spectrum of overlap between cardiovascular and oncologic diseases.
Jasrai Gill of Neptune City, New Jersey, is a cardiologist and chief medical officer. He specializes in cardiovascular disease and interventional cardiology. His experience and work scope covers multiple areas, including interventional cardiology, cardio-oncology, vascular medicine, drug development, and biotechnology. “Since cardio-oncology involves two medical fields,” Dr. Gill explains, “it requires a coordinated approach between cardiology and oncology physicians.”
What is Cardio-Oncology?

The purpose of cardio-oncology, according to Jasrai Gill, is to provide comprehensive care to cancer patients. This care covers everything from prevention to diagnosis and management of cardiotoxicity. “It’s not just heart failure that we focus on,” he adds, “but also everything from hypertension, cardiac arrhythmia, and vascular disease.”
The first mention of cardiovascular side effects as a result of radiotherapy and chemotherapy was in a study that was published over 50 years ago. But an aging population combined with a sharp increase of both cancer and cardiovascular patients led to the development of cardio-oncology as a field of medicine. To complicate things further from a medical point of view, it was observed that many cancer survivors had developed severe cases of cardiovascular diseases that contributed more to mortality than the cancer itself. Not just that, but recent studies have pointed to a higher risk among cancer patients who have pre-existing cardiovascular conditions. The toxic effects of cancer therapies are then superimposed on increased baseline cardiovascular risk.
Coordination and Collaboration
Such devastating side effects of both radiotherapy and chemotherapy required a whole new approach to cancer patients’ care. According to Jasrai Gill, some of those toxic side effects took years to develop and often times patients were lost to follow-up. This highlights the need for cancer survivors to be monitored for years under strict follow-up guidelines to detect early signs of cardiovascular diseases. In other words, there was a need for the two fields of medicine, oncology and cardiology, to collaborate, coordinate, and interact in a longitudinal way to provide adequate patient-focused care.
When patients received uncoordinated treatment from cardiologists and oncologists, the risk of toxic side effects increased. This made it all the more imperative for a team approach. Cardio-oncologists not only work on treating cancer, but also pay extra attention to preventive measures during the treatment to mitigate the high toxicity of cancer therapy agents. At the same time, these measures should not compromise the efficacy of the treatment.
Cardiac Arrhythmias
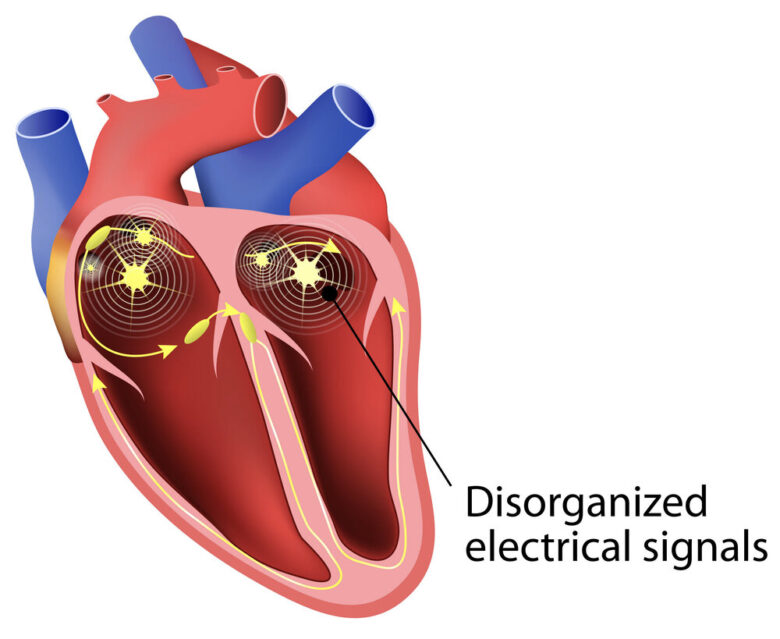
In recent years there has been an increase in cardiac arrhythmias among patients who were treated with anti-cancer medications. However, we still don’t know how these drugs play a role in or actually cause cardiac arrhythmias. Many factors contribute to the development of these conditions among cancer patients receiving treatment or prognosis, notes Jasrai Gill.
Cancer often causes certain metabolic changes and inflammation in the body of the patient which contribute to the development of cardiac arrhythmias. The type of therapy the patient receives might also increase their risk. In addition, patients with pre-existing cardiac diseases or those with multiple medical conditions are more likely to develop cardiac arrhythmias. This is especially true if the patients are aged 65 or older.
Cancer caused by cardiac arrhythmias is another example of the need for both cardiologists and oncologists to team up together during the treatment of patients at higher risk. When a cancer patient has a history of atrial fibrillation, a common arrhythmic problem, the care team approach allows for optimal assessment of therapeutic risk-benefit.
Cardiovascular Imaging and Cardio-Oncology
Cardiovascular imaging is an important part of the detection and treatment of conditions related to the toxic side effects of cancer therapies. Cardiovascular imaging is commonly used to screen and detect cardiotoxicity. It also helps gauge the patient’s response to the cancer treatment they’re undergoing, says Jasrai Gill.
Cardiovascular imaging is both easily accessible and safe to use. It has wide uses in detecting many cardiovascular conditions including valvular heart disease. The overlapping of both cancer and cardiovascular conditions here requires more cooperation between the relevant medical departments to create protocols related to screening, monitoring, and treating cardio-oncology patients. Representative imaging techniques include cardiac ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT). The protocols should also include surveillance of patients who are prone to developing complications long after the treatment.
Hypertension and Cancer

Many cancer patients develop treatment-related hypertension. The older the patient, the more likely they are to develop hypertension in this setting. Multiple novel targeted therapies act on pathways that are involved in control of blood pressure and vascular biology, according to Jasrai Gill, and disruption of these pathways can lead to side effects outside of their impact on the cancer.
Hypertension is serious health risk and needs to be aggressively managed in the setting of cancer therapy. In general, a multimodality approach to managing hypertension is necessary in cancer patients who are experiencing side effects from their chemotherapy. In addition to medical treatment, dietary and life-style modification are cornerstones to managing treatment-related hypertension.
Jasrai Gill on the Side Effects of Radiotherapy
While radiotherapy is considered an important component of cancer therapy for many patients, it carries well-known long term cardiovascular risks. According to Jasrai Gill, radiotherapy delivered to the chest, in particular to the left side, has the potential to have long term consequences to various structures within the heart, including the coronary arteries and heart valves. Additionally, radiation can be responsible for creating scars in the pericardium over time. However, radiotherapy has undergone many improvements including lowering the radiation doses and excluding the heart area from exposure to radiation.
Cardiology and oncology physicians have learned over the years that by working together and planning a coordinated approach to cancer treatment, they can prevent many cancer-related cardiovascular diseases.

